“Frozen shoulder”  is a term that is used when the shoulder becomes painful and loses motion because of inflammation. The tissues around the joint stiffen, scar tissue forms, and shoulder movements become difficult and painful.
is a term that is used when the shoulder becomes painful and loses motion because of inflammation. The tissues around the joint stiffen, scar tissue forms, and shoulder movements become difficult and painful.
The joint capsule of the shoulder joint has ligaments that hold the shoulder bones to each other. When the capsule becomes inflamed, the shoulder bones are unable to move freely in the joint. This pain prevents you from moving your arm. The lack of movement leads to stiffness and then even less motion. Over time, you will struggle to perform activities such as reaching over your head.
Frozen shoulder most commonly affects patients between the ages of 40 to 60 years old, and it is twice as common in women than in men. Also, patients who sustain a shoulder injury, or undergo surgery on the shoulder can develop a frozen shoulder joint.
If you have shoulder pain and stiffness and suspect you may have a frozen shoulder, contact your health care provider for proper diagnosis and treatment.
At Diversified Health you health care practitioner will make the diagnosis based on your symptoms and an examination of your shoulder. The main symptoms are decreased motion of the shoulder, pain, and stiffness.
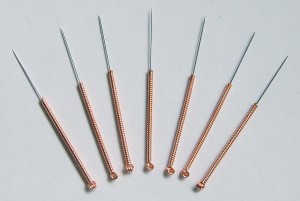
The goal of your practitioner is to release the scar tissue by bringing the shoulder through a full range of motion and to remove the scar tissue from the shoulder. Some of the therapies and modalities that will be used during your treatments are: Graston Technique, Cold Laser, T.E.N.S and Shockwave Therapy , Dry Needling, as well as a set of specific exercises and some time in our Rehab Gym.
Stretching exercises for frozen shoulder serves two functions: first to increase the motion in the joint and secondly to minimize the loss of muscle on the affected arm (muscle atrophy). The importance of stretching and exercises cannot be overemphasized as these are the key to successful frozen shoulder treatment.