Ah, summertime splendour. Nearly everyone’s favourite time of year in Victoria is met by longer days, lighter clothing and more casual footwear — namely, the all-too-common flip-flops. Unfortunately, while flip-flops may seem like a comfortable choice at first step, they can cause foot pain and exacerbate the following conditions. So, if you’re noticing aches and pains this time of year, and if flip-flops are part of your summertime routine, here’s what you need to know.
Why Flip-Flops Cause Foot Pain and Problems
Flip-flops lack support: and even if you don’t realize it, wearing flip-flops creates tension in the muscles of your feet and toes as the foot grips the flip-flop to prevent it from sliding off when walking.
Absent elevation: In addition, the lack of a slight heel elevation can cause excessive strain on your foot, calf muscles, and Achilles tendon. While, depending on your feet, not everyone requires a lot of support in their footwear, flip-flops’ complete lack of arch support and cushioning means your whole body absorbs the shock each time your feet strike the ground.
Standing and walking for long periods in flip-flops can cause or exacerbate underlying foot and postural conditions and cause pain that can interfere with your usual activities.
The Most Common Conditions Exacerbated by Flip-Flop Wearing
Plantar Fasciitis: Quite possibly the most common condition triggered by prolonged flip flop wearing, plantar fasciitis pain is often described as a burning or stabbing pain that’s felt in the heel or midsole of your foot. Plantar fasciitis pain results from inflammation of the plantar fascia, which can be caused by footwear lacking adequate arch support.
Flexor and Extensor Tendonitis: When you walk in flip-flops, your feet tense the muscles of your toes to stabilize the sole of the flip-flop. In addition, it’s also common to push off the ground from your big toe when walking in flip-flops. Over time, this can lead to strain and inflammation of the tendons responsible for flexing and extending your toes. The first signs and symptoms of flexor tendonitis and extensor tendonitis include pain along the top of the foot, under the big toe, or under your inner ankle when you walk, run, bend or straighten your toes.
Bunion Pain: If you have bunions, you know they can make a lot of different footwear off limits. And while flip flops appear as though they’d offer a reprieve from bunion pain caused by friction from narrow and enclosed footwear, the lack of cushioning under the big toe joint and ball of your foot can lead to inflammation, redness and pain.
Achilles Tendonitis Pain: Achilles tendonitis is caused when the tendon that runs between the back of your ankle and heel becomes strained, which can be triggered by wearing flat footwear without a slight heel elevation.
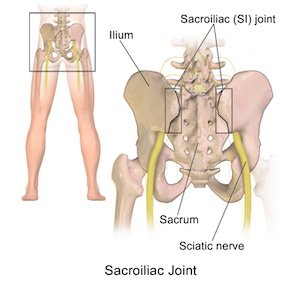
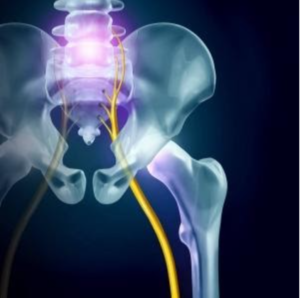
Knee, Hip or Lower Back Pain: Footwear that lacks adequate cushioning and support places unnecessary strain and impact on your ligaments and joints, which can cause inflammation and pain most commonly felt in the knees, hips and lower back.
Gait Issues, Postural Issues and Muscle Imbalances: Gait issues are prevalent and often go unnoticed until body aches and pains (or a sports injury) bring someone in for an assessment. Unaddressed gait issues can lead to muscle imbalances such as glute tightness that can cause an uneven tilt to the pelvis resulting in lower back and hip pain, nerve pain and joint issues. In addition, flat footwear such as flip-flops can interfere with the natural biomechanics of your feet, which, when unimpeded, help protect the body by absorbing shock, ensuring balance and maintaining body alignment.
Perhaps You Could Use a Little Support
Proper body alignment starts from the ground up: and sometimes something as minor as adjusting heel elevation and providing adequate arch support can make a big difference in helping to improve posture, relieve pain and correct movement patterns.
You don’t necessarily have to ditch your flip-flops altogether: reserve them for beach or short strolls in the yard. Even your most expensive running shoes or workboots may need a little tweaking to best support your feet and prevent foot pain and other complications.
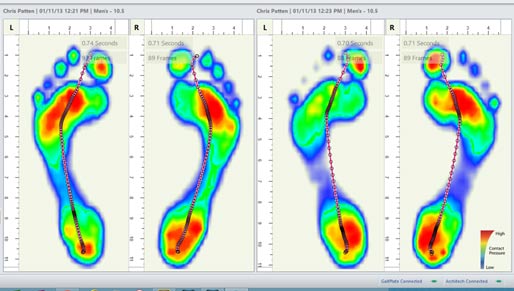
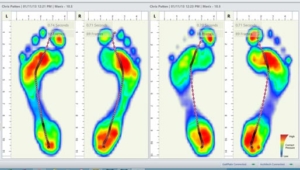
Custom orthotics that are tailored to your specific needs following a thorough GAIT analysis: can be easily inserted into different types of footwear. Adding orthotics to your everyday shoes and boots can help alleviate foot pain and correct gait issues by giving your feet the right amount of support where it’s needed. Custom orthotics can make a big difference in relieving foot pain and body aches caused by gait issues and suboptimal body alignment, resulting in more comfortable days on your feet.
If Foot Pain Persists
It never hurts to have things checked out by a health professional, and addressing the cause of foot pain early can prevent further injury and result in better overall outcomes.
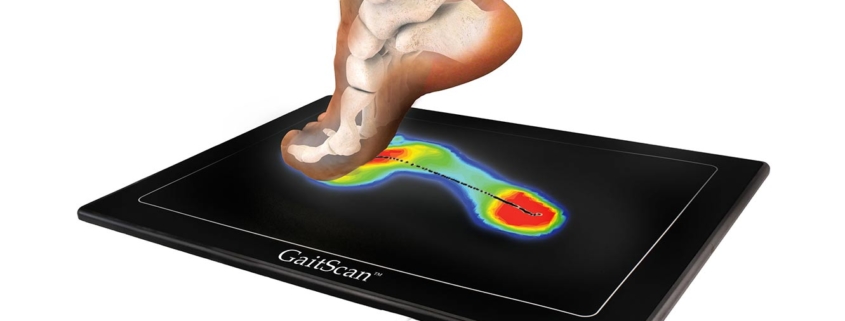
At Diversified Health Clinic, we use state-of-the-art GaitScan technology to accurately assess foot function and identify any imbalances, biomechanical issues and causes of pain. If faulty foot mechanics are found to be the cause of your pain, our practitioners can fit you with custom orthotic inserts that are specifically tailored for your feet. You can learn more about our comprehensive process here.
Take The Next Step Towards Happy, Healthy Feet
If foot pain, body aches or gait issues are slowing you down, our practitioners at Diversified Health can help. Take the first step on your road to recovery by booking an appointment with one of our practitioners today.
Call (250) 382-0018 or book an appointment online. We offer direct billing and weekday and weekend appointments. Please view our hours of operation and location details here.






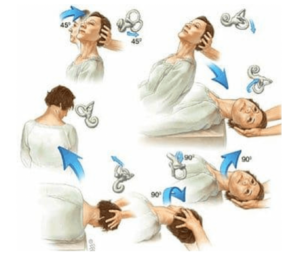
 intervention, or more persistent, requiring help from a health practitioner. Vertigo symptoms can also be intermittent, with many people experiencing what they refer to as “vertigo attacks” that come and go following activity or illness.
intervention, or more persistent, requiring help from a health practitioner. Vertigo symptoms can also be intermittent, with many people experiencing what they refer to as “vertigo attacks” that come and go following activity or illness. 







 Our multi-disciplinary team will work with you, with the ability to collaborate across treatment modalities to ensure you are getting the best treatment results. Our Diversified Health Team can evaluate, diagnose, and treat a wide range of conditions and injuries including:
Our multi-disciplinary team will work with you, with the ability to collaborate across treatment modalities to ensure you are getting the best treatment results. Our Diversified Health Team can evaluate, diagnose, and treat a wide range of conditions and injuries including:
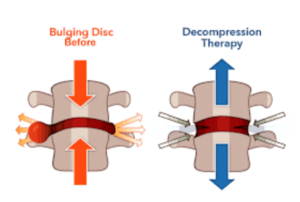
 If you have been struggling with chronic back, neck or sciatic pain, you do not have to live with the pain! spinal decompression therapy is a painless, non-surgical, drug-free way to help relieve chronic back, neck and sciatic pain. Continue reading to learn how spinal decompression works and why it’s an option worth exploring.
If you have been struggling with chronic back, neck or sciatic pain, you do not have to live with the pain! spinal decompression therapy is a painless, non-surgical, drug-free way to help relieve chronic back, neck and sciatic pain. Continue reading to learn how spinal decompression works and why it’s an option worth exploring. 



 Unlike off-the-shelf insoles and inserts, custom orthotics are created from exact molds of your feet that are taken after a thorough biomechanical assessment and Gait Analysis that examines your feet and posture when standing and walking. Making orthotics from an exact mold ensures the correction offered by your orthotics is just enough, providing support specifically where your feet need it without interfering with the healthy dynamics of your feet.
Unlike off-the-shelf insoles and inserts, custom orthotics are created from exact molds of your feet that are taken after a thorough biomechanical assessment and Gait Analysis that examines your feet and posture when standing and walking. Making orthotics from an exact mold ensures the correction offered by your orthotics is just enough, providing support specifically where your feet need it without interfering with the healthy dynamics of your feet.