 If you have been struggling with chronic back, neck or sciatic pain, you do not have to live with the pain! spinal decompression therapy is a painless, non-surgical, drug-free way to help relieve chronic back, neck and sciatic pain. Continue reading to learn how spinal decompression works and why it’s an option worth exploring.
If you have been struggling with chronic back, neck or sciatic pain, you do not have to live with the pain! spinal decompression therapy is a painless, non-surgical, drug-free way to help relieve chronic back, neck and sciatic pain. Continue reading to learn how spinal decompression works and why it’s an option worth exploring.
What is Spinal Decompression Therapy?
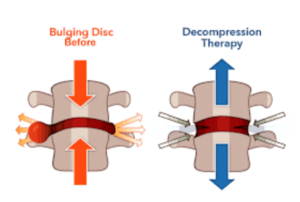
Non-surgical spinal decompression therapy utilizes a type of motorized traction that involves stretching the spine with the goal of relieving back pain and/or leg pain. The bones of the spine are slowly separated, and pressure is slowly reduced within the disc until a vacuum is formed. This vacuum creates negative pressure and space within the disc to allow disc fluid to move back into place. This reduces the bulge or herniation of the disc and creates an environment where the disc can receive more nutrients and therefore be able to heal more effectively.
Spinal Compression Is Used to Treat:

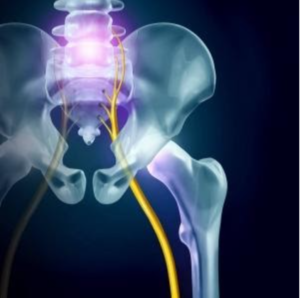
- Back, neck or sciatica pain
- Bulging or herniated disks
- Degenerative disk disease
- Worn Spinal Joints (posterior facet syndrome)
- Injured or diseased spinal nerve roots
When Do You Use Non-Surgical Spinal Decompression Therapy?
Spinal decompression therapy is for patients looking for a non-surgical and non-drug approach to relieving chronic back pain, sciatica, and spinal stenosis. Spinal decompression is also used for patients that present with an MRI that confirms herniated discs causing nerve pressure. However, spinal decompression treatments cannot be used for patients who are pregnant or suffering from spinal fractures, tumours of the spine, abdominal aortic aneurysm, severe osteoporotic disease, or metal implantations in their spine.
What Are Spinal Decompression Treatments Like?
During spinal decompression treatments, fully clothed patients are secured into a harness that is attached to the motorized table. The practitioner will program the table for your treatment and the amount of traction your spine will go through. Depending on the treatment, you will be lying either face-up or face down. Each session lasts no longer than 15-20 minutes. You will feel pressure applied to your lower back and will feel as though you are being “stretched out.” You should not feel any pain during spinal decompression therapy.
How Long Until You See Results?
Individual results vary; however, most patients notice a difference within their first 5-6 spinal decompression therapy treatments and experience pain relief within as few as 6-10 treatments.
Not only is spinal decompression painless – patients often enjoy the relief they feel from their symptoms when they are on the table being decompressed. Most patients will need to come in for treatment three times a week for one month, transitioning from passive to active treatments as their bodies respond and will also be prescribed a customized exercise program to target the areas that require more stabilization.
Clinical results show that spinal decompression has been effective in over 75% of patients treated. In addition, most patients found long-term relief or effective management of pain when they completed their spinal decompression treatments. Your practitioner may also recommend additional treatment modalities such as heat/cold therapy, electric stimulation, K-Laser and home exercises.
Benefits of Spinal Decompression Therapy
- Provides pain relief by relieving tension in tight, spasming or injured muscles. Spinal decompression helps to stimulate the nervous system to release neuro-chemical signals that have an analgesic effect on the body.
- Promotes the healing of spinal disc tissues by imposing a vacuum-like force on the spinal discs, which helps to draw healing fluids, cells, and other substances toward the damaged tissue.
- Helps restore normal spinal joint and disc alignment with the same vacuum-like force. That vacuum-like force helps to align the joints and discs which prevents further pain, inflammation, impaired mobility, and dysfunction.
- Relieves pressure on spinal nerves by increasing the space around the nerves which allows them to begin healing.
For More Information on Spinal Decompression Therapy (and Whether It’s Right for You):
Contact Diversified Health Clinic at 250-382-0018 to find out more about spinal decompression treatments, or book with our practitioners online at www.diversifiedhealth.janeapp.com
#physiotherapy #chiropractic #backpain #chronicbackpain #victoriabc #sciatica #degenerativedisc









 Leg pain can range from a mild irritation to an unbearable pain that makes it difficult to complete any day-to-day activities. Leg pain can take many different forms, from a dull ache to searing pain. Other symptoms that may also occur are a pins-and-needle sensation, numbness or weakness.
Leg pain can range from a mild irritation to an unbearable pain that makes it difficult to complete any day-to-day activities. Leg pain can take many different forms, from a dull ache to searing pain. Other symptoms that may also occur are a pins-and-needle sensation, numbness or weakness.

