Do you suffer from chronic pain or an old injury that interferes with your range of motion and the activities you enjoy? If so, physiotherapy accompanied by shockwave therapy treatments may be ideal for you. Shockwave therapy has been shown in studies to effectively reduce pain, break down old scar tissue and stimulate healing in stubborn injuries and joint pain without the cost or downtime of surgery. Continue reading to learn more about shockwave therapy’s many benefits.
What Is Shockwave Therapy?
Shockwave therapy is a non-surgical, non-invasive procedure whereby mechanical pulses of acoustic energy stimulate tissue repair, increase circulation, and help relieve pain where the treatment is applied. Physiotherapists may incorporate shockwave therapy as part of a patient’s injury rehabilitation treatment plan to help provide natural relief for acute or chronic pain and to stimulate the body’s natural healing response. In addition, shockwave therapy can be an excellent treatment for stubborn conditions or old injuries that haven’t responded well to other alternatives.
Conditions That Shockwave Therapy Treats
Shockwave therapy can be beneficial in many different applications but is especially helpful for treating muscle, ligament, tendon, bone and joint-related injuries and pain commonly associated with conditions including but not limited to:
- Rotator cuff injuries
- Stress fractures
- Tennis elbow (lateral epicondylitis)
- Golfer’s elbow (medial epicondylitis)
- Achilles tendinopathy
- Runner’s knee (patellofemoral pain syndrome)
- Jumper’s knee (patellar tendonitis)
- Calcified tendonitis
- Trigger finger
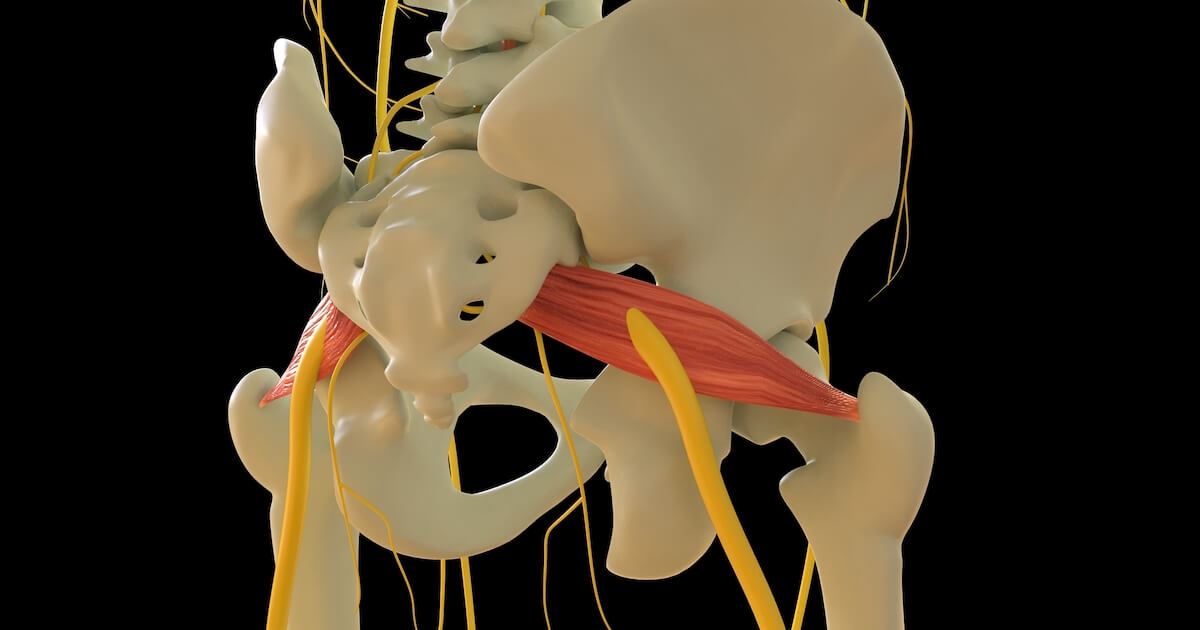
- Bursitis of the hip, knee, or shoulder
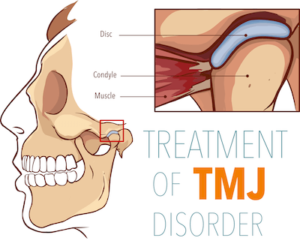
- TMJ disorders
- Shin splints
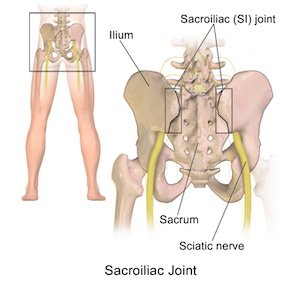
- Back pain
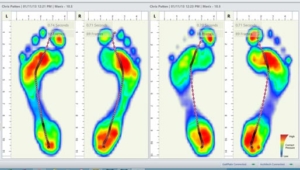
- Plantar fasciitis
- Shoulder/rotator cuff tendinitis
- Overuse strains and sprains
- Injuries caused by accidents
- Chronic muscle tension and pain
What to Expect From Shockwave Therapy Treatments
After assessing your condition and devising a treatment plan, your physiotherapist will start your treatment by applying a cool conductive gel (similar to ultrasound jelly) to the area being treated so that the handpiece used to deliver the acoustic energy pulses can easily be maneuvered. Treatments usually take around 15 minutes and are typically carried out a week apart.
What does it feel like?
Topical numbing agents, painkillers and anti-inflammatories are not required during shockwave therapy and are discouraged because they can interfere with shockwave therapy’s inflammatory response, which initiates tissue regeneration and healing. Shockwave therapy treatments typically feel like dull pulsing sensations in the tissues being treated. Treatment discomfort depends on the intensity of the treatment and the tenderness of the area being treated but is usually tolerable, and your physiotherapist can adjust the intensity to ensure your comfort. You may feel slight tingly sensations, warmth or tenderness in the treated area for up to a few days following treatment while the tissue’s healing response occurs.
Is there any downtime?
The beauty of undergoing non-invasive shockwave therapy treatments is how you can resume light activity following your treatments. Your physiotherapist will, however, ask you to avoid any rigorous or strenuous activity for two or more days following treatment, depending on your condition. You may also experience slight swelling or tenderness in the area treated for a few days following your procedure. Inflammation following your shockwave treatments is normal and indicative of the healing process taking place.
How many treatments will I need to see results?
Some patients notice pain reduction following their first treatment, with improved healing and pain relief as treatments progress. Shockwave treatment plans typically consist of 3 to 6 sessions spaced one or more weeks apart. Your physiotherapist will tailor a treatment plan ideal for your specific condition and requirements.
Find Out Whether Shockwave Therapy Is Right for You!
Don’t ignore pain. Start the healing process today by booking your appointment with one of our expert physiotherapists. Call Diversified Health Clinic at (250) 382-0018 or book an appointment online.










 intervention, or more persistent, requiring help from a health practitioner. Vertigo symptoms can also be intermittent, with many people experiencing what they refer to as “vertigo attacks” that come and go following activity or illness.
intervention, or more persistent, requiring help from a health practitioner. Vertigo symptoms can also be intermittent, with many people experiencing what they refer to as “vertigo attacks” that come and go following activity or illness. 

 Jennifer completed her Master’s of Physical Therapy at
Jennifer completed her Master’s of Physical Therapy at