“What Causes Vertigo?” It’s a question we receive a lot at our clinic. The dizzy, spinny and falling symptoms can feel nauseating and interfere with your sleep and daily activities. The good news is that benign paroxysmal positional vertigo, or BPPV (the most common type), can be easily assessed and treated, resulting in immediate and lasting relief.
First, What Is Vertigo?
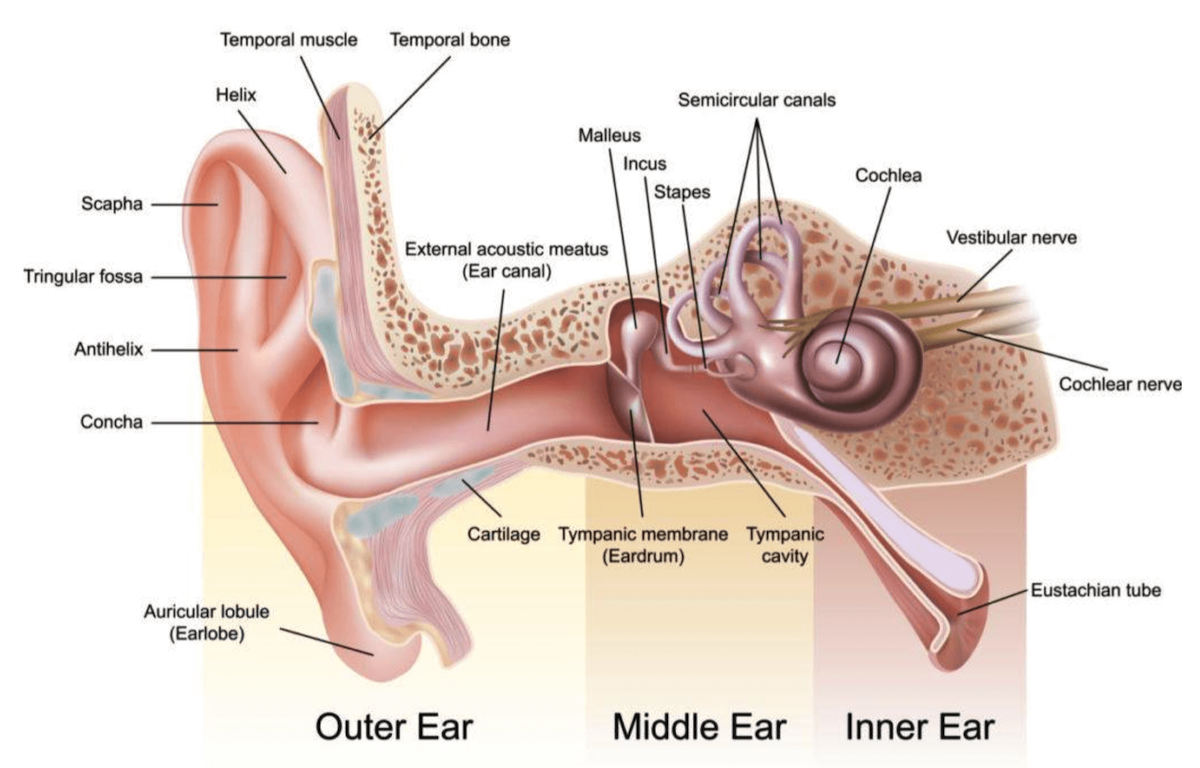
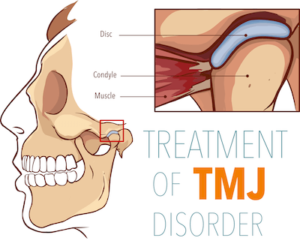
Vertigo is the term used to describe the sensation of moving or spinning when you are stationary. Vertigo is the symptom of an inner ear condition that results when tiny calcium carbonate crystals (canaliths) located in the utricle portion of your inner ear (that help control balance) shift out of place, causing the sensation of dizziness or motion.
Vertigo symptoms can range from slight to severe and be fleeting, quickly resolving without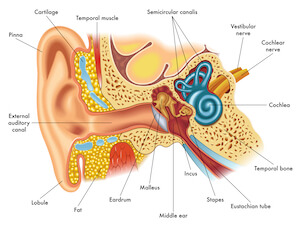 intervention, or more persistent, requiring help from a health practitioner. Vertigo symptoms can also be intermittent, with many people experiencing what they refer to as “vertigo attacks” that come and go following activity or illness.
intervention, or more persistent, requiring help from a health practitioner. Vertigo symptoms can also be intermittent, with many people experiencing what they refer to as “vertigo attacks” that come and go following activity or illness.
There are two primary types of vertigo as follows, and while they share things in common, each may have different causative factors and require different treatment approaches.
Central Vertigo
Central vertigo is caused by an underlying condition such as Meniere’s disease, infection, or brain injury that affects the central vestibular structures (brainstem cerebellum, vestibular apparatus).
Central vertigo typically presents as more pronounced and prolonged or as recurrent vertigo attacks that can last for several hours and are accompanied by other symptoms, including migraine headaches, nausea, tinnitus, hearing loss and the sensation of one or both ears feeling blocked. Central vertigo can also be so severe that suffers cannot walk or balance themselves. Treatment depends on causative factors.
Peripheral Vertigo
Otherwise known as benign paroxysmal positional vertigo (BPPV), peripheral vertigo is the most common type, accounting for over 90% of all causes of vertigo. Peripheral vertigo occurs when activities and head movement disrupt the crystals of the inner ear (the peripheral vestibular system).
Peripheral vertigo symptoms can be slight or severe and last only a few seconds, a few days, several weeks, or be recurrent. Recurrent and prolonged episodes of vertigo can be triggered by several factors, some of which are similar to central vertigo. However, peripheral vertigo is when the cause of vertigo is isolated to disruption of the inner ear instead of being related to another underlying condition or head injury.
When Vertigo Requires Emergency Attention
Vertigo symptoms accompanied by fever, pain, confusion, slurred speech, vision changes, or stupor require immediate medical attention to rule out potentially serious conditions.
What Causes Vertigo? Common Triggers
Sudden, recurrent and prolonged episodes of peripheral vertigo can be triggered by a number of factors, some of which are similar to central vertigo. The most common vertigo triggers include:
- Shifts in head movement that can be as simple as rolling over in bed or tilting your head back and forward (head banging movements at rock concerts is one extreme example of head movements that can trigger a vertigo episode)
- Following exposure to irregular movements, including being on a boat in rilling waves or following a ride at the fair
- Head movements during leisure and athletic activities
- A sudden blow to the head or a sudden shift in head movement due to impact
- Head and neck injuries
- Direct injury or infection of the vestibular system of the inner ear
- Certain medications
- Migraines
- Age and hereditary factors
- Fluctuation hormones, especially during the first trimester of pregnancy
- Viral ear infections
- Metabolic changes or nutrient deficiencies, including a lack of Vitamin D and calcium
- (Aural vertigo) Cold water entering the ears when swimming or diving
- (Alternobaric vertigo) Imbalanced ear pressure when ascending or descending while scuba diving
- Allergies
- Cardiovascular disease
- Anxiety
- Neurological disorders
- Viral infections
- Vestibular dysfunction
- Vascular conditions
- Multiple Sclerosis
What Causes Vertigo to Go Away on Its Own?
For some people, vertigo episodes that are slight and fleeting often disappear as quickly as they appear and resolve without medical treatment. Vertigo that resolves on its own can be a bout of motion sickness or a movement that causes the previously disrupted crystals of the inner ear to shift back into place.
When Vertigo Doesn’t Resolve on Its Own
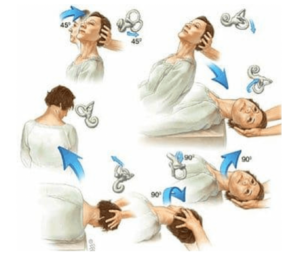
When vertigo symptoms become more bothersome, severe, recurrent or lingers, treatment is sought and sometimes necessary to relieve vertigo symptoms and prevent them from interfering with daily life and leisure. Treatment often involves specific head positioning maneuvers and exercises that help the calcium carbonate crystals of the inner ear to readjust and move back to their proper position.
What to Do When Vertigo Symptoms Arise
While vertigo may not be entirely preventable, there are things you can do to manage the severity of vertigo symptoms when they occur.
- Immediately sit or lay down when you feel dizzy.
- Sleep and nap with head slightly elevated.
- Avoid stretching your neck when reaching for something.
- Avoid tilting your head forward when bending over to pick things up — keep your head aligned as you squat to pick items up instead.
- Move your head slowly during activity.
- When getting up from laying down, rise slowly and stabilize yourself with something if you feel dizzy.
- Always use handrails when taking stairs and escalators.
- Utilize calming breathing techniques to avoid anxiousness.
- Make an appointment with your GP if severe symptoms are accompanied by other symptoms such as headache, vision changes, confusion or fever.
- Seek vertigo treatment with a local health practitioner such as our physiotherapist Jennifer Mildon and our chiropractor Doctor Caitlan Sellan at Diversified Health Clinic, located in downtown Victoria.
Effective Treatments for Relieving Vertigo in Victoria, B.C.
When vertigo symptoms strike, treatment can help. At Diversified Health Clinic, one our Physiotherapists, Jennifer Mildon, and one of our Chiropractors, Dr. Cailtan Sellan, both have a special interest and training in vestibular rehabilitation and vertigo treatments. You’ll be happy to know that benign paroxysmal positional vertigo (BPPV) is easy to assess and treat, often with only a few vestibular rehab sessions that can be performed whether or not you’re immediately experiencing vertigo symptoms.
What to Expect from Vestibular Rehab Treatments
Your first session will include a thorough assessment followed by a series of manual repositioning techniques that help the crystals of your inner ear settle into their proper position. You’ll also be given personalized vestibular exercises you can perform at home between treatments to improve your balance and decrease vertigo symptoms when they occur.
Book Your Vertigo Assessment and Treatment Today
To arrange for an assessment and vertigo treatment, please call our clinic at (250) 382-0018 and request a vestibular session with Jennifer Mildon or Dr. Caitlan Sellan. You can also book online here.
If you have questions about whether our vestibular rehab treatments are right for you, contact our clinic to request a free, no-obligation, 5-minute consultation.
Important
On the day of your treatment, we kindly ask that you arrange travel plans so that you will not have to drive home after your session, and you are welcome to bring a friend or family member with you to your appointment.




 Jennifer completed her Master’s of Physical Therapy at
Jennifer completed her Master’s of Physical Therapy at 












 Delayed onset muscle soreness is more pronounced when:
Delayed onset muscle soreness is more pronounced when: