 In the last decade, vibration training was mainly used in the fitness industry, but the use of vibration equipment has now expanded and is widely used in physical therapy, rehabilitation, professional sports, and is increasingly used in beauty and wellness applications. There is an abundance of research worldwide that highlights the benefits of Whole Body Vibration. Studies have shown remarkable results for improved fitness and health in a fraction of the time, compared to traditional exercise.
In the last decade, vibration training was mainly used in the fitness industry, but the use of vibration equipment has now expanded and is widely used in physical therapy, rehabilitation, professional sports, and is increasingly used in beauty and wellness applications. There is an abundance of research worldwide that highlights the benefits of Whole Body Vibration. Studies have shown remarkable results for improved fitness and health in a fraction of the time, compared to traditional exercise.
How vibration machines work
Whole body vibration is implemented through the use of a vibrating platform on which static poses are held or dynamic exercises can be performed depending on the type and force of the machine. The vibrations are generated by a complex mechanism underneath the platform, and those vibrations improve flexibility/balance and strengthens bones/muscles.
Bone Strength
Loss of bone density affects many people at different age groups. One of the key benefits of Whole Body Vibration is that it can stimulate the release of natural hormones. These hormones can in many cases stop the loss of bone density and in some situations may even reverse the effects of osteoporosis. These beneficial claims are from the ground breaking study reported in the Journal of Bone and Mineral Research in 2006.
Blood circulation
Increasing blood circulation can be beneficial in so many ways. With increased blood circulation, your cells receive more oxygen and nourishment. White blood cells help remove debris from broken down cells and from toxins that enter the body. The increase of the body’s lymphatic drainage system is a great way to improve overall health and strengthen the immune system.
Muscles
Regular use of our whole body vibration training machines can help exercise your muscles by increasing the force on the muscles. This is done without the damaging impact of traditional exercise on your joints. There is also little to no strain on ligaments and tendons when one uses a whole body vibration machine correctly.
Pain
Muscle, joint, and nerve pain are all debilitating problems that affect millions of people. Many whole body vibration machines have programs and exercises that help develop your core strength which can improve posture. A stronger core helps to eliminate the root of many muscle related ailments. Strengthening bones and muscle will also help to reduce muscle aches and pain.
At Diversified Health, our physiotherapists and chiropractors use a vibration machine as a rehabilitation tool. Vibration training can help strengthen muscles without putting strain on joints and ligaments. Rehabilitation often involves an increase in blood flow which is one of the keys to repairing and regenerating soft tissue. Improved circulation also helps to drain fluid build-up from injured tissue.

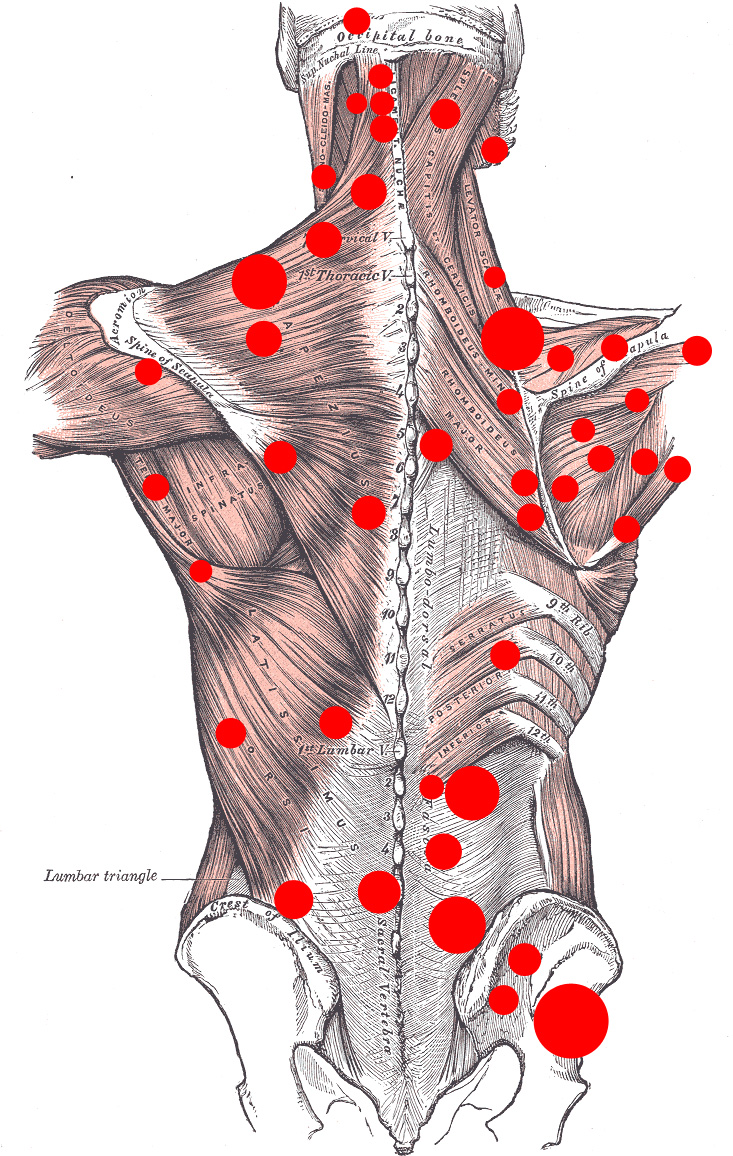 Myofascial pain syndrome is a chronic musculoskeletal pain disorder that can involve either a single muscle or a muscle group. It refers to pain and
Myofascial pain syndrome is a chronic musculoskeletal pain disorder that can involve either a single muscle or a muscle group. It refers to pain and Trigger point dry needling, also referred to as intramuscular stimulation (IMS) and/or intramuscular therapy (IMT) is an invasive procedure in which an acupuncture needle is inserted into the skin and muscle.
Trigger point dry needling, also referred to as intramuscular stimulation (IMS) and/or intramuscular therapy (IMT) is an invasive procedure in which an acupuncture needle is inserted into the skin and muscle. 

 Bursitis is typically identified by localized pain or swelling. Bursitis occurs when the small sac (bursa) found inside joints becomes inflamed. The fluid-filled sac helps to lubricate and cushion the joint. When it is inflamed, movement can be painful. Usually bursitis occurs in larger joints such as shoulders and hips.
Bursitis is typically identified by localized pain or swelling. Bursitis occurs when the small sac (bursa) found inside joints becomes inflamed. The fluid-filled sac helps to lubricate and cushion the joint. When it is inflamed, movement can be painful. Usually bursitis occurs in larger joints such as shoulders and hips.


